This is part of our Medicaid Concepts series, in which we try to provide a high level overview of key concepts in the Medicaid industry today.
Latest interviews
Topic overview
What do we mean by jail health?
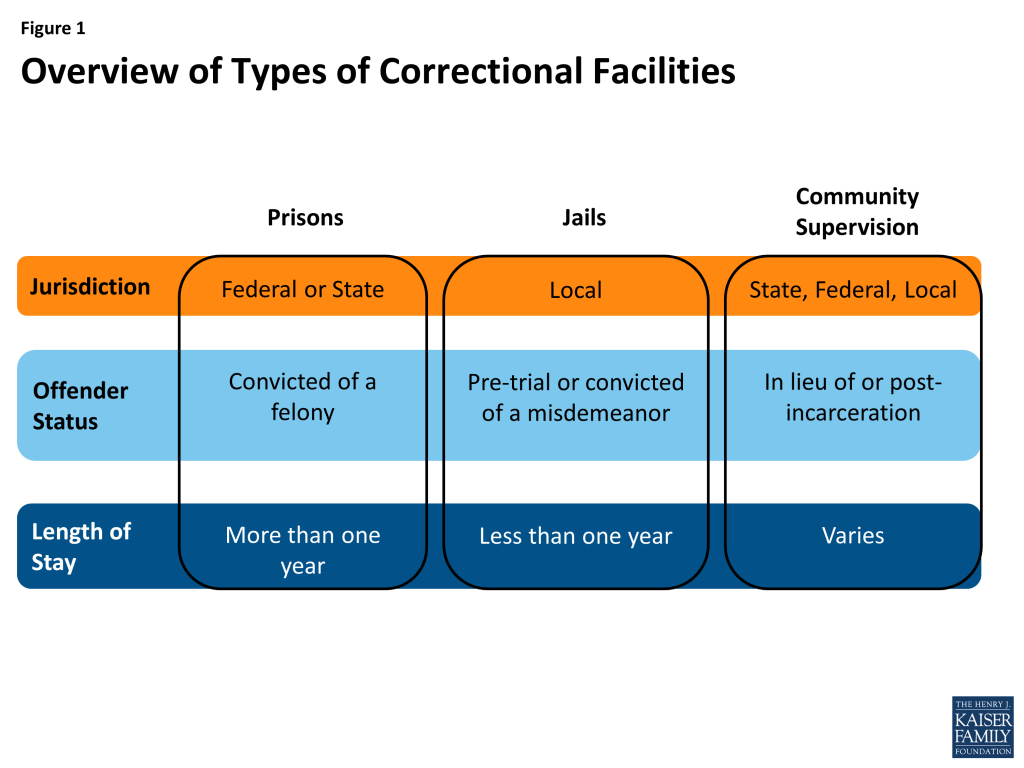
In general this discussion includes both healthcare services while incarcerated and during the transition period once the individual leaves prison and returns to society. While incarcerated, there are a range of services and contractors who provide physical and mental health services to prisoners. When offenders exit prison, there are programs operated by health plans and states to assist in the transition.
What role does Medicaid play in this area?
Medicaid can cover services for inmates and returning offenders. Before the Affordable Care Act in 2014 (ACA) many states did not choose to provide services to inmates under Medicaid because they usually did not meet eligibility criteria (non-disabled adults without dependent children). ACA provided new funding via the “expansion” group category that made it easier for prisoners to be eligible while inside.
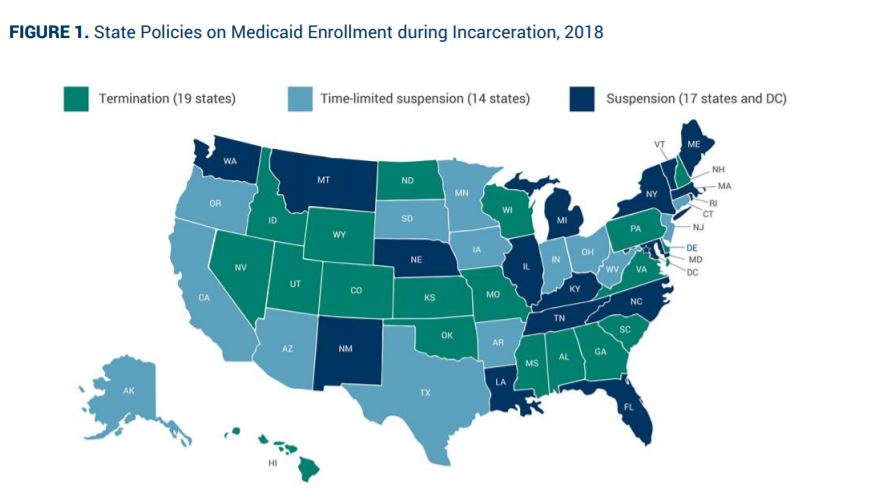
Many states follow CMS guidance on suspending (vs terminating) inmate coverage once they enter prison. This allows the state to more easily resume coverage once the offender returns (which is a critical time period of transition, with much higher changes of mortality and other negative outcomes). This also allows for Medicaid to cover off-site healthcare services such as inpatient stays, even when the inmate goes back to prison after the stay.
States that do cover eligible prisoners usually exclude them from managed care capitation arrangements (instead covering them under their fee for service program).
States and health plans continue to try and improve the healthcare services provided to incarcerated and returning members. For returning members, Medicaid programs and plans focus on provider coordination, job services and closing gaps related to social determinants of health.
Explore further
https://www.naco.org/resources/medicaid-coverage-and-county-jails
https://www.macpac.gov/wp-content/uploads/2018/07/Medicaid-and-the-Criminal-Justice-System.pdf
https://www.disabilitybenefitscenter.org/faq/health-insurance-in-prison