This is part of our Medicaid Concepts series, in which we provide a high level overview of key concepts in the Medicaid industry today.
What do we mean by Modularity?
States spend billions of dollars each year on claims payment and related technology systems. These payments have traditionally gone to a handful of vendors able to build such large scale solutions.
It has proven difficult to flexibly evolve Medicaid technology systems when most functions reside in one solution. Over the past 20 years, CMS (which pays for the majority of the costs of these systems) has attempted to create positive disruption with an emphasis on modularity. In lay person’s terms, this means using a set of smaller modules that can work together to accomplish objectives instead of one monolithic system.
An entire industry has grown up around the concept of modularity, including both technology and consulting vendors.
To understand modularity, there are two related key terms:
MMIS– Medicaid Management Information Systems is the term used to talk about the technology systems needed to pay provider claims, conduct certain federally required functions (like fraud detection) and interface with other systems such as eligibility and enrollment. This term is defined in section 1903 of the Social Security Act. At the most simple level, states must have payment systems approved by CMS since CMS is paying so much of the costs of healthcare services.
MITA – The Medicaid Information Technology Architecture (MITA) initiative is sponsored by CMS and is designed to improve systems used in Medicaid programs. It has various goals and standards, and states have to report on their use of related principles in their system design.
One of the common concerns is perceived lack of precision in the definitions provided by CMS. Many stakeholders have called for CMS to identify a list of acceptable modules.
“A module is a packaged, functional business process or set of processes implemented through software, data, and interoperable interfaces that are enabled through design principles in which functions of a complex system are partitioned into discrete, scalable, reusable components. An MMIS module is a discrete piece (component) of software that can be used to implement an MMIS business area as defined in the Medicaid Enterprise Certification Toolkit (MECT)” – CMS State Medicaid Director Letter, August 16, 2016
What role does Medicaid play?
While CMS pays most of the costs of these systems, states procure them. As states update their MMIS systems, they have an opportunity to do a modular procurement. So far, states have typically sought to procure modules for claims payment, eligibility, drug management and electronic visit verification. In addition to modules, states also procure Systems Integrator (SI) contracts. SI vendors provide the overarching system needed to integrate modules together.
Explore further
https://www.medicaid.gov/medicaid/data-systems/medicaid-management-information-system/index.html
https://www.medicaid.gov/medicaid/data-systems/medicaid-information-technology-architecture/index.html
https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidInfoTechArch/Downloads/mitaoverview.pdf
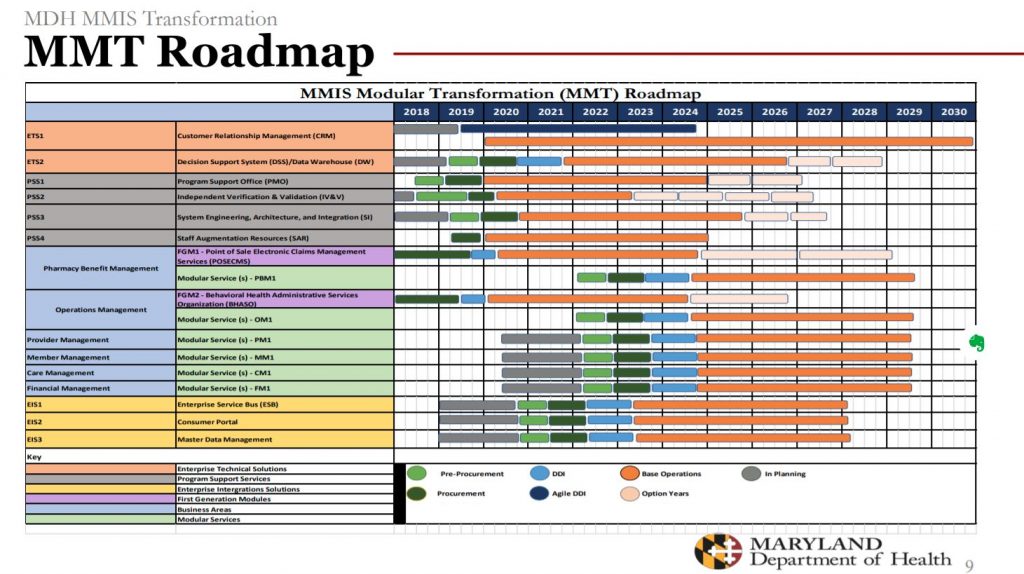
https://mmcp.health.maryland.gov/Documents/MMAC/2019/05_May/2019%20MMAC%20Summit_MMIS%20Transformation.pdf
https://doit.maryland.gov/contracts/Documents/catsPlus_torfp_status/M00B0600019-MHT-MMT-RFP.pdf
https://www.cns-inc.com/wp-content/uploads/2018/06/CNSI-Modularity-White-Paper-FINAL_0.pdf
https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/contracting/pre-solicitation-announcement.pdf
https://www.medicaid.gov/medicaid/data-systems/downloads/rfi-modular.pdf
https://www.medicaid.gov/medicaid/data-systems/medicaid-enterprise-certification-toolkit/index.html
https://downloads.conduent.com/content/usa/en/white-paper/defining-mmis-modularity.pdf
https://www.optum.com/content/dam/optum3/optum/en/resources/PDFs/optum-modularity-approach-for-hhs-medicaid.pdf
https://www.medicaid.gov/federal-policy-guidance/downloads/smd16010.pdf
https://www2.deloitte.com/us/en/pages/public-sector/solutions/medicaid-management-information-system-modernization.html