MM Curator summary
[MM Curator Summary]: The money is there, the referral system is in place- there’s just not enough actual houses.
By Clarissa Donnelly-DeRoven
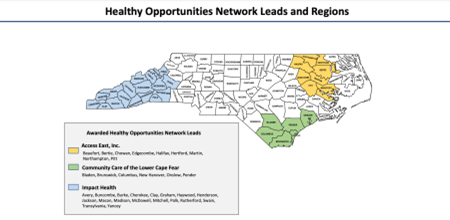
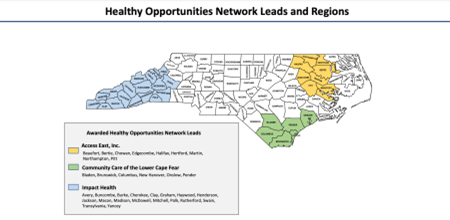
North Carolina’s state Medicaid office is sending millions of dollars to organizations that help people with housing, domestic violence, and other chronically stressful situations.
By paying these agencies to help people on Medicaid with extreme life stressors, the state hopes it can help those same people avoid illness and in the process save money that would otherwise be spent on health care.
The project, called the Healthy Opportunities Pilot, or HOP, began its three-phase roll out in March after years of planning. It started with services to reduce hunger, which many say are going pretty well. In May, the pilot began funding housing and transportation services. In June, the state planned to begin reimbursing organizations that deal with domestic violence.
Some portions of the project have been stalled, though.
Researchers have long documented the ways that extremely stressful situations, such as homelessness and domestic violence, impact mental and physical health. The last two decades have also brought research showing how these events can wreak havoc on the mind and body.
Experiencing and coping with stress is a critical part of human development. Stress – in moderate amounts – is designed to keep us safe. The so-called “fight or flight” response causes the heart to start beating faster, blood vessels to restrict to more quickly push blood, oxygen, and other nutrients throughout the body. We make hormones – like adrenaline – that can give the energy needed to fight, flight, or flee. Our immune system turns up its inflammatory response.
As the body tunnels all its energy into overcoming a stressful situation, it diverts resources from other energy-intensive bodily processes, such as reproduction and the part of the brain that deals with decision-making and controlling emotions.
Over short periods of time, the response works. But if it never turns off — which is what happens when you’re constantly worried about where you’ll sleep, or if your partner will put you in the hospital again — that’s where problems start.
A heart pumping too hard for too long can cause vascular disease, high blood pressure, and increase the likelihood of a heart attack. Too many stress hormones can exacerbate conditions like diabetes, while reproductive hormones needed to sustain a healthy pregnancy can struggle to turn back on after being suppressed for too long.
An overactive inflammatory response can lead to the suppression of the immune system — so rather than stress causing sickness, it stops a body from being able to fight off diseases as effectively. Brains can even begin to “rewire,” building up the parts that deal with the threat response, while ignoring the parts that deal with complex problem solving.
Paying someone’s rent is no good if there’s no houses
No other state has ever attempted a project like Healthy Opportunities before, and so there’s been a fair amount of growing pains, from issues with the referral process, to a lack of information about the pilot for Medicaid recipients.
Some of the issues the pilot is facing are more issue specific — the state-wide housing shortage, for one.
Amy Upham is the executive director of the Buncombe County’s Eleanor Health Foundation, an organization helping people with substance use disorder and other mental illnesses connect with transportation, housing, affordable medications, employment, and more.
“We’re ready. We’ve got staff. We’ve got reserves where we can front the cost until we get reimbursed by Medicaid,” Upham said. “We’ve got all the resource lists for housing. We are able to house someone.”
But, she added, “Is there a place to put them? No.”
“We’re finding that there’s not a lot of housing available in Murphy,” said Charam Miller, the director of Macon Program for Promise. “I feel like it’s just a struggle for all of Western North Carolina right now to find safe, affordable housing.”
Those experiences are echoed by research done by the National Association of Realtors, which found that post-pandemic, housing prices across the U.S. rose by about 30 percent, even as the inventory of homes for sale dropped to record lows in 2021.
At a roundtable discussion hosted by the Duke Margolis Center in July, officials from different agencies involved in the project acknowledged the scope of this issue.
“When we think about housing, we have a strain in our housing system,” said LaQuana Palmer, who works with the platform NCCARE 360 through which all the program referrals happen.
Even with their expertise and funding, some HOP providers have been struggling to find places for Medicaid recipients in need to live. Other organizations have successfully helped only a handful of Medicaid patients, either through getting them on a housing waitlist or helping them with their utility bills.
Then there’s the paperwork: housing sustainability plans, inspections and other federal requirements.
“We can’t even find them a place to live, let alone that they’re gonna want to jump through all these hoops or that the landlord’s gonna want to jump through all these hoops to house this person,” Upham said.
“Housing services, in particular, have been one of the more challenging types of services for us to implement,” said Amanda Van Vleet, the associate director of innovation at NC Medicaid who oversees the pilot. “The really challenging part there, the core of it, really gets to integrating non-medical services into the Medicaid program.”
Getting paid by reimbursements, rather than grants, is new for many of the participating organizations. And the process is more cumbersome because the federal Centers for Medicare and Medicaid Services has strict documentation rules for providers that haven’t participated in Medicaid before — which, for the Healthy Opportunities Pilot, is all of the organizations.
“We are proposing modifications to that right now to try to eliminate what we can while still having enough program integrity in place, but making it a little bit more doable and manageable for the [organizations],” Van Vleet said.
Privacy concerns complicate help for domestic violence survivors
Despite the challenges, housing services are actually starting to get up and running.
Domestic violence services are a different story. This part of the pilot was supposed to begin its roll out in June, but it didn’t, and the state doesn’t have a timeline for when it will begin.
The first challenge comes from strict federal privacy laws around handling information and data about domestic violence survivors. These laws are often major funding sources for domestic violence agencies, and they impose limitations on how client information can be shared, and with whom.
For the purposes of the HOP project, the state is treating domestic violence survivors as Medicaid patients, but that’s tricky.
“A health plan, for example, will need to know who received the service and if they’re a covered member of theirs so that they can pay for their services,” Van Vleet said. “They also need to know exactly what service that person received in order to reimburse for it.”
The state and domestic violence agencies realized that these needs conflict with each other, but it seems they underestimated how complicated they would be to disentangle.
“That’s the fundamental tension that we’ve been dealing with, is kind of how we’re able to make both of those things work,” Van Vleet said.
There are technical changes that need to be made to the NC CARE 360 referral platform in order to comply with federal privacy regulations. Those have to be made by the company Unite Us, which contracts with the state to run the platform.
In a statement, Unite Us said they’re working with state officials and advocates to protect survivors while allowing service providers to get paid.
Contracts between the state and every organization participating in the pilot also need to be updated to include stipulations about data gathering and sharing. And anyone in the program who deals with participants’ data will need to undergo training about domestic violence, privacy, and data security.
“Because receiving domestic violence services is such a delicate topic, survivors need to be aware of who will know that they have qualified for these services,” said Kathleen Lockwood, the policy director at the North Carolina Coalition Against Domestic Violence, an organization that’s pushed the state around best practices for years.
Each agency in an individual case needs to be mindful of survivor safety. The clearest way this comes up, Lockwood explained, is in contact preferences. For example, if somebody says not to call them or leave a message, that request must be respected — for many, it could be a matter of life or death.
“We anticipate a survivor accessing services through the Healthy Opportunities Program versus through interacting with their domestic service provider in the community to be receiving a very similar if not the same experience,” Lockwood said.
A stop-gap solution
Organizations have been creating privacy workarounds, explained Jennifer Turner-Lynn, the assistant director at REACH of Macon County, an organization that supports survivors of domestic violence and plans to participate in the pilot.
“When a client comes to us, and we believe they qualify for services, we discuss those service options with them,” she said. “If they are interested… we have them sign a release of information. We assist them in contacting Medicaid.”
Once they reach their Medicaid case manager, they’ll be referred to another organization in the pilot. Then the client tells that organization they want to receive services through REACH.
“Our staff completes the service, provides the assistance, and places notes in the system, but never at any point stipulates this person is a ‘victim’; because it’s in [the other organization’s] system,” Turner-Lynn said. “It will look just like any client they serve as it’s under their umbrella, not ours.”
The other human service organization bills Medicaid and then pays REACH after receiving payment.
“There is only one person, outside of REACH, who ever knows that this person qualifies as a victim, and that’s the key point person at the contracted [human service organization] with whom they talk with immediately,” she said.
It’s definitely roundabout, she said, but so far it’s worked. Those in the field hope the problems will be resolved soon, so they can start providing services and have the effectiveness of their services be evaluated.
“From our perspective any data — however long the span or however short the span — that can show the linkages between health and safety in the domestic violence realm will be valuable data,” Lockwood said.
“The correlation or causation between receiving services and later health outcomes are really going to make the case for communities to continue to invest in domestic violence services.”
Clipped from: https://www.northcarolinahealthnews.org/2022/09/08/new-housing-program-faces-hurdles/