
MM Curator summary
Oklahoma now will get a lot more federal funding than it originally planned when it chose to expand last year.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
Two COVID-19 relief packages passed by Congress feature increases in Medicaid funding for the state of Oklahoma. (Pablo Angulo)
The Oklahoma Legislature’s appropriations chairmen are set to meet this morning with Oklahoma Health Care Authority staff about how additional federal Medicaid funding authorized by Congress and held by OHCA could affect next year’s state budget. The complicated situation stands as a potential X-factor for state leaders tasked with paying for Medicaid expansion, third-party managed Medicaid and a bevy of other budget items.
“It’s a significant amount of money,” OHCA chief financial officer Aaron Morris said. “I wouldn’t say we have completely sat on it. We’ve had a few initiatives we have introduced and continued to introduce. We’ve also returned funds to other state agencies that participate in the Medicaid program. We’ve returned funds to our hospital partners who pay SHOPP.”
The state’s Supplemental Hospital Offset Payment Program (SHOPP) charges certain hospitals a fee that is used to maximize the state’s drawdown of federal Medicaid dollars. Known as SoonerCare in Oklahoma, Medicaid is a federal-state partnership that provides health insurance to low-income children, families and disabled individuals. The portion of a state’s Medicaid program paid by federal money is determined by the Federal Medical Assistance Percentage, or FMAP, which changes annually in an inverse relationship to a state’s economic strength.
Since January 2020, states have received an additional 6.2 percent for its FMAP base rate under a provision of the Families First Coronavirus Relief Act. Between January and June 2020, Morris said that increase sent about $150 million to the Oklahoma Health Care Authority and other state agencies. Morris said he did not know how much money the boosted FMAP has brought in since July, but he said the OHCA’s cash on hand from the enhanced rate “likely exceeds $100 million.”
The 6.2 percent enhanced FMAP will continue for the duration of the federal public health emergency declaration, which currently runs through April.
“My guess is we will hear a decision either in late March or early April about whether that (public health emergency declaration) is renewed for another 90 days,” Morris said.
But wait, there’s more money
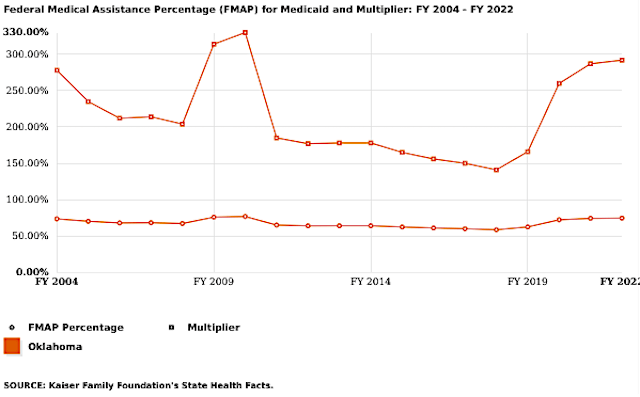
The Federal Medical Assistance Percentage, called FMAP, fluctuates annually in an inverse relationship to the strength of a state’s economy. (Kaiser Family Foundation)
Whether the 6.2 percent FMAP enhancement continues or not, Oklahoma is also poised to pick up a separate 5 percent FMAP bump starting July 1 when the state expands Medicaid to cover low-income adults. That provision was included in Congress’ latest COVID-19 relief package, the American Rescue Plan, and is specifically for states that have not yet adopted Medicaid expansion from the Obama-era Affordable Care Act.
While Oklahoma voters approved State Question 802 in 2020 to expand Medicaid, the constitutional amendment established a July 1 deadline for implementation, meaning Oklahoma will receive the 5 percent FMAP increase for eight financial quarters, or two years.
“That’s a 6.2 percent (increase) plus a 5 percent (increase) on top of our base FMAP,” Morris said. “So it’s an interesting time period that we’ve never really experienced before.”
Asked about the situation Tuesday, Gov. Kevin Stitt also used the word “interesting.”
“There could be some extra money inside of the Health Care Authority,” Stitt said. “So that’s interesting.”
The Legislature’s budget leaders are also intrigued.
“I just have a whole lot of questions,” said House Appropriations and Budget Chairman Kevin Wallace (R-Wellston).
Wallace, Senate Appropriations and Budget Chairman Roger Thompson (R-Okemah) and others met in Wallace’s office Tuesday to discuss the FY 2022 budget, which they must finalize before the end of May. Thompson noted that a state’s FMAP rate decreases when its economy performs better.
“The Oklahoma economy is doing very well, so I [expect] the FMAP to be going down in the next cycle,” Thompson said. “So I think we need to be saving some of this FMAP money we have today into our FMAP savings account so that when that rate drops, our (health care) providers are not hurt.”
Thompson rejected the notion that additional FMAP dollars could be used to fund Medicaid expansion, which will require about $164 million from the state Legislature. The federal government covers 90 percent of costs for a state’s expansion population.
“We’re still looking at the number. We’re still at $164 million until we find out otherwise,” Thompson said. “From a budgeting perspective, even though the feds are giving us extra money, whatever that number is it doesn’t matter. It’s still going to be one-time money, and our position is still we don’t use one-time money to pay for an ongoing expense. So we’ve got to figure out a way to pay that number with the funds that we have that would be reoccuring funds.”
Wallace agreed.
“We definitely don’t want to fund the expansion with one-time money,” he said.
Last year, lawmakers passed a bill that would have brought in about $134 million to fund Medicaid expansion by increasing the SHOPP fee, but Gov. Kevin Stitt vetoed the bill. It is unclear whether the Legislature intends to unveil and pass a similar SHOPP fee increase to fund Medicaid expansion this year.
“I would say all things are still in discussion,” Wallace said. “I don’t believe there are any final decisions that have been made yet.”
Wallace said it is important for lawmakers to have a good grasp of agency accounts because the Legislature is constitutionally tasked with the power of the purse.
“The last thing we want [an agency] to do is start some sort of programing where, when the federal dollars run out, they come back to the Legislature and say, ‘We need more money,'” Wallace said.
House Appropriations and Budget Chairman Kevin Wallace (R-Wellston) speaks to media Monday, March 9, 2020. (Tres Savage)
Managed care funding question looms as well
Complicating the Legislature’s decisions on how to fund Medicaid is the disagreement over third-party management of the state’s SoonerCare program. The OHCA has already signed contracts with a slate of private insurance companies that are expected to begin managing Medicaid patients’ care this summer, unless the Legislature takes some sort of action to block implementation, such as not funding the roughly $50 million estimated start-up cost.
Thompson said the additional FMAP dollars could come into play for that budget item.
“I don’t mind using $50 million of that federal money or what we are sitting on from the enhanced FMAP because that’s a one-time expense moving people over into that managed care,” he said.
House Speaker Charles McCall (R-Atoka) said the amount of FMAP money available is an important variable for legislative budget leaders.
“This is definitely something that very much will be a driver in terms of what the impact is on our budget that we’re crafting right now for health care,” McCall said. “We know we are going to fund [Medicaid expansion]. The people of the state of Oklahoma have mandated it. But if the amount that we have to come up with this year is lower because of the stimulus package, that’s great because it gives us a little more time to figure out the longterm funding of the program. In the short term, we’re going to be able to fund it. In the long term, there will be some tougher decisions to make down the road, I suspect.”
Another complicating factor for OHCA could turn into a difficult decision once the federal public health emergency declaration ends and the 6.2 percent FMAP increase terminates. In order to qualify for that increase during the pandemic, states had to agree not to disenroll Medicaid members for reasons other than death or relocation to another state.
As a result, Morris said Oklahoma’s Medicaid population has climbed from around 800,000 to about 960,000.
“Typically we’re looking at how they qualify,” Morris said. “If their income goes above the threshold, in a normal circumstance they would become ineligible for Medicaid, but during the public health emergency, as a stipulation of accepting the 6.2 percent advanced (rate), we can’t disenroll those folks.”
Clipped from: https://nondoc.com/2021/03/24/federal-relief-bills-will-send-oklahoma-more-medicaid-money/
