MM Curator summary
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
[MM Curator Summary]: The author wants to be ticked about expansion but also wants to benefit from the idea that lockdowns caused a surge in MH needs. Besides all that we get some decent data on MH drug trends in Idaho.
Clipped from: https://idahofreedom.org/mental-health-declines-as-medicaid-funds-record-psychotropic-drug-use/
Taxpayer-subsidized government healthcare is not making people healthier.
New data shows that the use of psychotropic drugs among Medicaid beneficiaries is projected to reach an all-time high for the third consecutive year. With one in every five Medicaid prescriptions in Idaho written for these drugs, there exists a serious problem with mental health throughout the Gem State.
Psychotropic drugs are generally used to treat mental health conditions like anxiety, depression and mood disorders. In 2016, there were just under 400,000 claims for such medications. Since then, the use of these drugs has increased significantly, with claims growing 86% as of 2021. Estimates for 2022 say that Idaho Medicaid will spend $91 million to cover just short of one million claims for psychotropics by the end of the year.
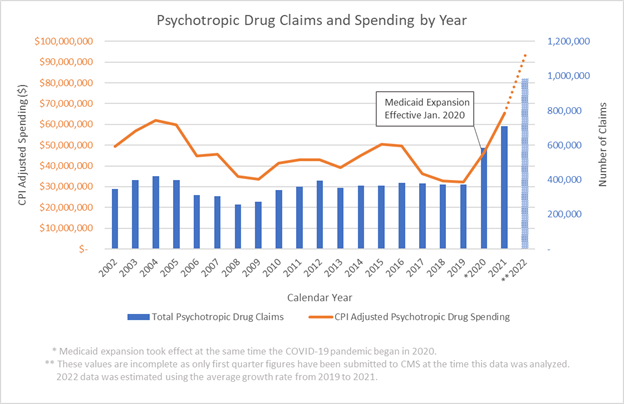
Figure 1
Medicaid expansion and the COVID-19 pandemic both started in early 2020, as did the steep increase in psychotropic use. In the previous decade, spending on psychotropic medications declined by 5% per year and the number of prescriptions declined by 1% per year, when adjusted for inflation and Medicaid enrollment. Since 2020, however, this decline suddenly became a sharp annualized increase of 6% in prescriptions and 15% in spending (see Figure 2).
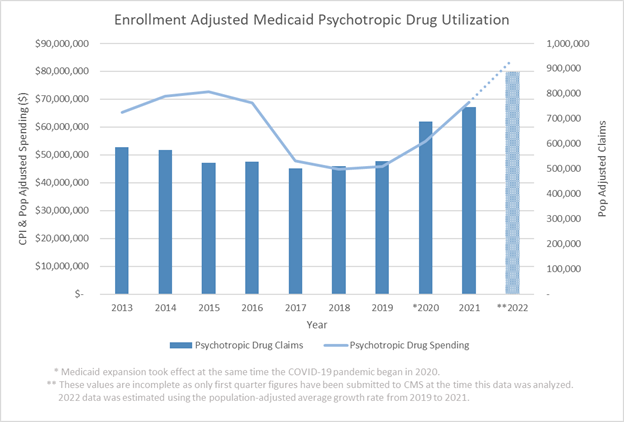
Figure 2
Medicaid expansion added to the number of people who could receive benefits. But that change alone does not explain the rapid increase in prescriptions and prescription expenses. Demographic changes played a key role.
The effects of the pandemic – exacerbated by harsh government policies, including Gov. Brad Little’s statewide lockdowns – created a surge of Idahoans applying for Medicaid. For adults under 40 and those in their 60s, lockdown policies created isolation, unemployment, and economic hardship, all of which harmed their mental health significantly more than was the case for all other age groups. This likely generated a demographic shift necessary, among both existing and new Medicaid enrollees, that accounts for the sudden rise in psychotropic drug use. Despite the state’s relatively quick economic recovery touted by the governor, these concerning trends remain and are worsening.
There is cause for skepticism about the efficacy of prescribing psychotropic drugs to treat mental health conditions. One groundbreaking study asserts that the foundational theory supporting antidepressants – the chemical imbalance theory – is incorrect. Naturally, this research also calls into question whether antidepressants are effective forms of treatment. This theory has also been the basis of hesitancy for doctors and patients to stop antidepressant treatments, leading to lifelong use by people who would otherwise be able to seek better alternatives.
Despite doubts about the efficacy of some psychotropics, like antidepressants, these types of drugs are still commonly overprescribed. A national study notes that three out of every five visits where a new psychotropic drug was prescribed to a patient had no corresponding psychiatric diagnosis. Not only is this practice potentially detrimental to patient health, but the same study links this over-prescription to rising costs within the Medicaid system.
This tendency to overprescribe psychotropic drugs also made it common for patients to be taking more than one of these medications at the same time. Disturbingly, patients on Medicaid are significantly more likely to be taking multiple psychotropic drugs, despite this being an ill-advised practice that could have harmful effects on patients. This is especially concerning for the case in Idaho, as the state ranks among those with the highest incidence of this practice.
What is happening within the Medicaid system is an example of how government control negatively impacts people’s lives. The big government policies that dictated how we weathered the pandemic destroyed the livelihoods of many Idahoans and had long-term negative effects on their health and freedom.
The entrapment of patients in chronic therapies is a common convention of modern medicine. Guaranteeing that patients continue their treatments without the hurdle of paying for them – as the Medicaid system does so well – is good for business among medical interest groups. Some healthcare professionals are beginning to notice these practices, resulting in the increasing popularity of osteopathic physicians versus their allopathic counterparts – that is, DOs rather than MDs. Scholars are finding that not only are mental health conditions not treated well with medications, but lifestyle plays a greater role in mental health than originally thought, and the medical community is beginning to take note.
Patients should be weary of those claiming to advocate for their well-being, only to call for bigger government and more social programs. Like subsidies and bailouts to support companies that are failing due to their bad business models, Medicaid is subsidizing the use of healthcare treatments and practices that may not be best for patients. However, the consequences of doing so are more severe than traditional business bailouts and the result is a worse healthcare system for everyone.
