MM Curator summary
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
[MM Curator Summary]: Its almost as if there are a few Billion rea$on$ the national MCOs are pushing all the chicken littles to squawk. I mean rea$on$ besides their altruistic, Fortune 100 little hearts.
Total Medicaid and CHIP enrollment is now over 90 million. The latest national Medicaid managed care enrollment data (from 2020) show 72% of Medicaid beneficiaries were enrolled in comprehensive managed care organizations (MCOs). In FY 2021, payments to comprehensive Medicaid MCOs accounted for 52% of total Medicaid spending (or more than $376 billion). Medicaid is a major source of revenue and profits for multi-state insurance companies. KFF analysis of National Association of Insurance Commissioners (NAIC) data show gross margins per enrollee in the Medicaid managed care market were higher in 2021 than they were pre-pandemic. Medicaid MCOs have played a key role in responding to the COVID-19 pandemic and are expected to work with states in conducting outreach and providing support to enrollees during the “unwinding” of the continuous enrollment requirement. Beginning April 1, 2023, states were able to restart disenrollments (which had been paused since February 2020) after conducting a full review of eligibility. Many people will likely be found to be no longer eligible for Medicaid, while others could face administrative barriers and lose coverage despite remaining eligible. Medicaid MCOs have a financial interest in maintaining enrollment, which could also prevent disruptions in care for enrollees. This brief takes a closer look at the five largest publicly traded companies (also referred to as “parent” firms) operating Medicaid MCOs which account for half of Medicaid MCO enrollment nationally. Information and data reported in this brief come from quarterly company earnings reports, financial filings, and other company materials as well as from national administrative data.
Medicaid enrollment in the five largest publicly traded companies operating Medicaid MCOs
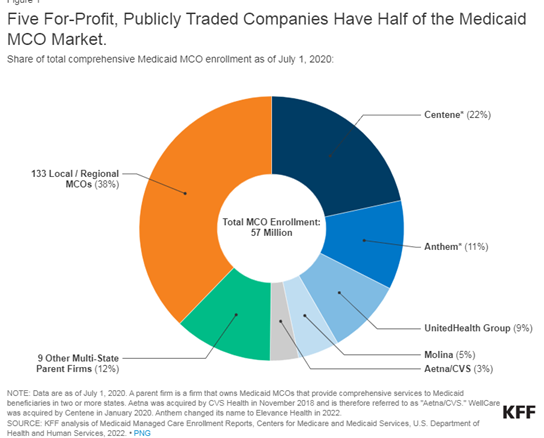
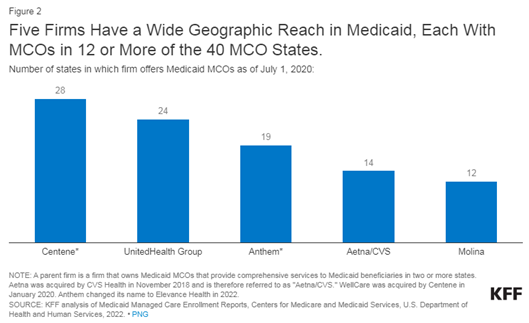
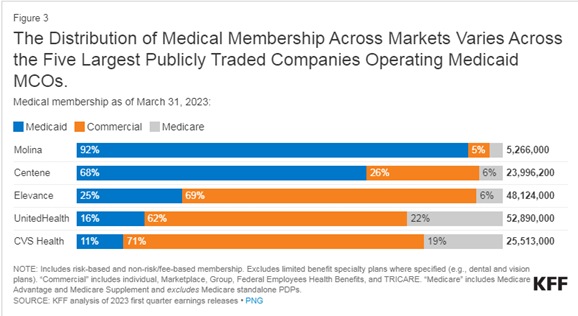
Five for-profit, publicly traded companies – Centene, Elevance (formerly Anthem), UnitedHealth Group, Molina, and CVS Health – account for 50% of Medicaid MCO enrollment nationally (Figure 1). All five are ranked in the Fortune 500, and four are ranked in the top 100, with total revenues that ranged from $32 billion (Molina) to $324 billion (UnitedHealth Group) for 2022. Each company operates Medicaid MCOs in 12 or more states (Figure 2). All five firms also operate in the commercial and Medicare markets (Figure 3); however, the distribution of membership across markets varies across firms. Two firms – Molina and Centene– have historically focused predominantly on the Medicaid market. Medicaid members accounted for over 90% of Molina’s overall medical membership and nearly 70% of Centene’s medical membership as of March 2023 (Figure 3).
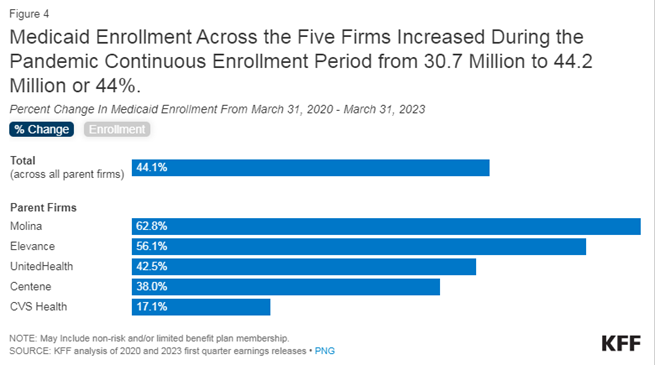
Combined Medicaid enrollment across the five firms increased by 13.5 million or 44.1% from March 2020 to March 2023 (Figure 4). Medicaid enrollment overall grew by more than 20 million (or about 31%) during the continuous enrollment period (February 2020 to January 2023), resulting in growth in MCO enrollment as well. Enrollment growth has been primarily attributed to the Families First Coronavirus Response Act (FFCRA) provision that required states to ensure continuous enrollment for Medicaid enrollees in exchange for a temporary increase in the Medicaid match rate. Growth in parent firm Medicaid enrollment may also reflect other activity including firm acquisitions and/or new contracts. For the firms that report this information, Medicaid revenue growth 2022 over 2021 ranged from 11% (Centene) to 18% (UnitedHealth) to 21% (Molina). These same firms reported Medicaid revenue growth ranging from 13% (Centene) to 16% (UnitedHealth) to 43% (Molina) year-over-year 2021 over 2020. Molina reported the medical margin earned by the Medicaid segment was $3.0 billion in 2022 and $2.3 billion in 2021 (medical margin = premium revenue – medical costs).
Implications of “unwinding” for the five largest publicly traded companies operating Medicaid MCOs
All five firms expect Medicaid enrollment losses following the end of the continuous enrollment requirement (over 2023 and 2024); however, firms expect to retain some members who lose Medicaid coverage in their Marketplace and other products (Appendix Table). The Consolidated Appropriations Act, 2023 ended the continuous enrollment provision and allowed states to resume disenrollments starting April 1, 2023. While the number of Medicaid enrollees who may be disenrolled during the unwinding period is highly uncertain, it is estimated that millions will lose coverage. KFF estimates 17 million people could lose Medicaid coverage – including some who are no longer eligible and others who are still eligible but face administrative barriers to renewal. Rates of Medicaid coverage loss will vary across states depending on how states approach unwinding. CMS has issued specific guidance allowing states to permit MCOs to update enrollee contact information and conduct outreach about the eligibility renewal process to facilitate continued enrollment as well as Marketplace transitions, where appropriate. In June 2023, CMS released new guidance highlighting several new strategies available to states to prevent procedural terminations including permitting managed care plans to assist enrollees in completing certain parts of renewal forms.
In first quarter 2023 investor earnings calls, executives of the publicly traded companies operating Medicaid MCOs expressed the aim of maximizing continuity of coverage for members through supporting continued enrollment in Medicaid and transitions to the Marketplace (and other products), where appropriate. The firms report conducting direct and indirect outreach, including text messages, live calls, and community-based provider campaigns, to educate members about Medicaid redeterminations and the renewal process as well as about their Marketplace options if they are no longer eligible for Medicaid (Appendix Table).
All five firms offer a Qualified Health Plan (QHP) in the ACA marketplace in many states where they operate a Medicaid MCO, however there may not be plan alignment if plans operate regionally. Current enrollees who are determined to no longer be eligible for Medicaid may be eligible for ACA marketplace (which has higher income eligibility thresholds than Medicaid) or other coverage (e.g., CHIP coverage or employer sponsored insurance (ESI)). Individuals eligible for coverage in the Marketplace may qualify for plans with zero premiums; however, individuals transitioning to Marketplace coverage may face higher cost-sharing and different provider networks. Prior analyses suggest that individuals face barriers moving from Medicaid to other coverage programs and many may experience gaps in coverage. CMS guidance outlines states may encourage MCOs that also offer a QHP to share information with their own enrollees who have been determined ineligible for Medicaid to assist in the transfer of individuals to Marketplace coverage (as long as state-specific laws and/or contract requirements do not prohibit this activity). To avoid gaps in coverage, managed care plans may reach out to individuals before they lose coverage to allow them to apply for Marketplace coverage in advance.
Looking Ahead
Medicaid managed care plans have a financial interest in maintaining enrollment, which could also prevent disruptions in care for enrollees. The five publicly traded firms that are the subject of this analysis account for half of all Medicaid MCO enrollment nationally. As states unwind the continuous enrollment provision, many people will likely be found to be no longer eligible for Medicaid. Others could face administrative barriers and lose coverage despite remaining eligible. Medicaid managed care plans can assist state Medicaid agencies in communicating with enrollees, conducting outreach and assistance, and ultimately, in improving coverage retention – including facilitating transitions to the Marketplace.