MM Curator summary
The state hospital association has gathered enough signatures for its version of the voter Medicaid expansion ballot initiative.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
PBS NewsHour
Voters will decide whether to expand Medicaid to more low-income South Dakotans as long as the secretary of state verifies enough petition signatures were turned in on Monday.
South Dakotans Decide Healthcare said it turned in 46,119 signatures from registered South Dakota voters. That’s more than the 33,921-signature threshold needed for initiated constitutional amendments to be placed on the November 2022 ballot.
The number “really shows the grassroots energy and excitement around this,” said spokesman Zach Marcus.
South Dakotans Decide Healthcare was the only group to turn in its proposed ballot question ahead of Monday’s deadline for initiated constitutional amendments. Initiated measures have a later deadline.
Medicaid is a federal-state health insurance program for low-income people. South Dakota is one of 12 states that has not accepted federal incentives to expand Medicaid eligibility, according to the Kaiser Family Foundation.
Medicaid expansion has only failed once when put before voters, according to Health Affairs. Voters in Maine, Idaho, Utah, Nebraska, Oklahoma and Missouri approved expansion. Montanans rejected expansion — which would have been covered through a tobacco tax increase — but lawmakers later approved it.
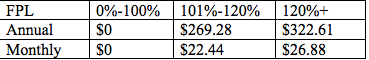
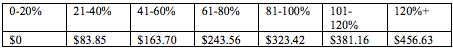
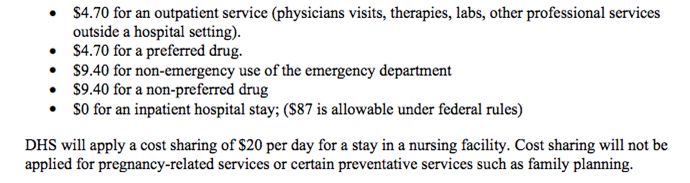
The South Dakota amendment would expand Medicaid to people between 18 and 65 who earn 133% or less of the federal poverty level.
Expansion would make Medicaid available to 42,500 additional South Dakotans in its first year, according to the non-partisan Legislative Research Council.
Studies show Medicaid expansion improves healthcare outcomes while producing economic benefits for recipients, healthcare systems and the overall economy.
Medicaid expansion faces a challenge after the Legislature voted in 2020 to refer a constitutional amendment to the voters during the June 2022 election — before the Medicaid vote in November 2022.
The proposed amendment says any ballot question that raises taxes or spends at least $10 million — such as the Medicaid expansion question — must be approved by 60%, not 50%, of the voters.
Sen. Lee Schoenbeck, R-Watertown, supports the amendment.
Schoenbeck “acknowledged that his expedited push was motivated by the Medicaid expansion campaign, but argued the vote threshold should apply to all ballot initiatives that levy taxes or spend significant state funds,” according to the Associated Press.
Expansion supporters are concerned about voter turnout in the June election since it’s a primary election without a presidential race. Just 26% of South Dakota voters participated in the June 2018 election compared to 65% in November.
“When we educate voters on why this is going to be helpful for South Dakota, when we educate voters on why this matters and will help them and their families, South Dakota voters respond to this,” Marcus said. “So if we need to get 60% of the vote for this to pass, that’s what we’ll do.”
South Dakotans Decide Healthcare is a statewide ballot question committee that raised $21,639 by the start of 2021, records show. Donors include the AARP, Farmers Union, healthcare organizations and the Fairness Project, a D.C.-based social and economic justice nonprofit.
Proposed initiated amendments that won’t be on the ballot addressed redistricting and elections. Those groups did not turn in petitions Monday, according to the secretary of state. A proposed initiated measure for recreational marijuana and an initiated measure that also addresses Medicaid expansion have a May 3 deadline.
Clipped from: https://listen.sdpb.org/healthcare/2021-11-08/sd-medicaid-expansion-to-appear-on-2022-election-ballot-pending-validation