Many of our clients are part of efforts to further integration of behavioral health and physical health care in a variety of different structures across the country. Whether you are a plan that is part of a state transformation effort, examining the potential for integration as a driver for quality improvement or working with providers to develop value-based payment for integrated care, there is a tremendous amount activity in this area.
Reading Time: 7 minutes
Intended Readers: Plan Executive Level Staff and integration solution providers
Key Topics: Environments, Categories of integration efforts, Operational components
Environments
The landscape of integrated care in states is varied and dynamic. There are many states that have already moved to integrate responsibility for behavioral health and physical health at the plan or community care organization level. Some others are taking steps in this direction and still others have not started to move on this particular area yet, but could begin the process at any time.
The most direct route for states to incentivize integration in their Medicaid programs is to procure the services together from a single integrated health plan. However, it is not the only way states are trying to advance integrated efforts. Some are acknowledging that there are populations within the integration effort that may benefit from special focus in a carve-out or similar structure. There are also states that have not taken concrete steps to structurally incentivize integrated care but are using existing contracts to push inclusion of all member issues in developing care plans and treatment.
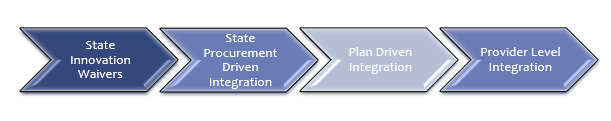
Plans have to operate within the environment of the state(s) where they work. Is this state integrating behavioral health and physical health in its procurement of services? Is this state still managing the behavioral health and physical health in different plans or structures, but expecting plans to work together to advance larger goals? Is there no expectation for integration at the plan level, but, instead, opportunity for plans to work to advance integration at the provider level?
Category 1 – State Innovation Waivers (1915i)
States can bring integration efforts into the state through the use of Medicaid innovation waivers that allow them to leverage more creative payment structures to support the integration of behavioral health and physical health. Many states have done work in this area that has advanced the knowledge-base for integrated health services and identified potential avenues for further integration.
California is the most familiar example of a state pushing integration efforts through state transformation and Medicaid waivers. The CalAIM initiative is attempting to drive more integrated care, along with a combination of other initiatives. Currently, the state has a county-managed system with four different types of models. Those models do not easily facilitate integrated care, particularly when it comes to people with serious mental illness or substance use disorders.
Category 2 – State Procurement Driven Integration (1915c)
Several states have advanced integration through the procurement of health plans that are responsible for both the delivery of physical health and behavioral health services. These efforts give states direct levers to drive change and give plans flexibility in how they manage the various components of service delivery to ensure that costs remain manageable and outcomes are improved for their members.
Ohio and North Carolina have taken this procurement-driven approach in recent years, developing different delivery models, but both attempting to improve outcomes for members with behavioral health and physical health challenges and breaking down of silos between the service delivery systems. In Ohio, all behavioral helath services are now part of the responsibilities for the same plans that were previously managing physical health services. In their most recent procurement, Ohio also added a separate program to manage multi-needs children.
The State of North Carolina has gone through an extensive evolution of the management of behavioral health services – from a county-driven system, that is still in place in many states, to a regional “local managing entity” structure that brought together counties and leveraged the economies of scale, to those LME-MCOs merging and consolidating over the years, to a new model that will bring most behavioral health services under the same managed care plans who manage physical health, but individuals with more complicated behavioral health challenges being managed by “tailored” plans.
Plans that are operating under models where the state is attempting to integrate service management into its procurement of plan services have a clearer picture of what is expected and ability to deliver because of the dollars being included in the PMPM. These plans have to understand that the behavioral health provider networks are not on the same level as physical health provider networks in terms of sophistication of clinical service planning, electronic health records, documentation and claims processing. These integrated plans have the opportunity to help professionalize the behavioral health provider networks, but there is investment needed to support that work.
Category 3 – Plan Driven Integration Efforts
Plans have incentives beyond state priorities and contracts to drive integration efforts. Barriers to access, network management, utilization management and quality can also drive a need for better integrated care. These plan driven efforts can be identified through quality improvement efforts, contract compliance efforts or work in data analytics that identifies populations who are experiencing challenges that could be prevented with a more integrated service delivery system.
Category 4 – Facilitating and Supporting Provider Level Integration Efforts
At the level closest to members, plans are piloting a variety of initiatives to better coordinate and integrate care for behavioral health and physical health with hospitals, health systems, Federally Qualified Health Centers and Certified Community Behavioral Health providers. These pilot projects demonstrate a return on investment and show the value of integration in a concrete, tangible manner.
Operational Components
All of the operational areas within a plan can and should be involved in integration efforts, from the call center, to the care coordination team, utilization management, quality improvement, provider network management, data and information technology. All areas of plan operations have something to contribute to integration efforts.
How A Plan Can Enhance Its Efforts Toward Integration of Behavioral Health and Physical Health Services
Besides your own research into this topic, there are a few key tactics that can help you overcome the most common challenges related to integration of physical and behavioral health services. If our services and expertise are a fit for your needs as you develop or execute your strategy, engaging with us is a simple process. If we are not the right fit, we are happy to make a referral to another firm who may be:
- Better understand the state environment for your plan – What waivers has the state requested? What waivers have been approved? What is the procurement cycle? What are the governor and legislature discussing when it comes to Medicaid? Are there other drivers for integration?
- Surface concerns your team has around integration and barriers that have been experienced in trying to advance integration efforts – An integrated care project will impact current workflows and business organization approaches. An initial listening-session series can save you a lot of time and mistakes.
- Identify projects that could advance integration in your health plan that also solve other challenges within the plan – pilots with providers, data analytics efforts and analysis of member journeys and experience – When you get into a full-scale integration project, small-wins will be important to establish momentum. And alignment with multiple objectives will be key to sustain success.
